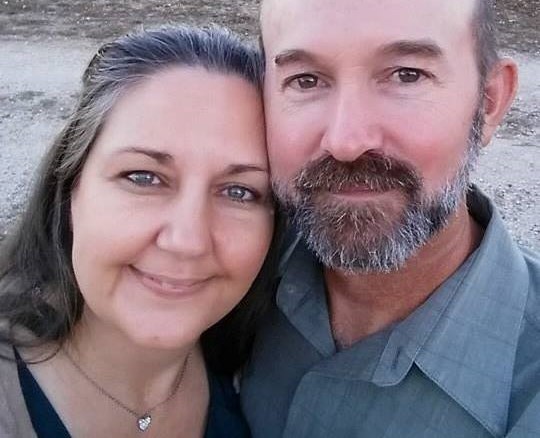
Deborah Smithey, CPM
Senior Midwife
I am Deborah Smithey, nationally certified by the North American Registry of Midwives as a Certified Professional Midwife (CPM). I maintain certification by the American Heart Association in Neonatal Resuscitation as well as Adult and Infant Basic Life Support (CPR). But none of that qualifies me to be your midwife. Only you can choose the right midwife for you.
I rely on my hands and simple tools for most routine examinations, reserving the use of technology to assist only when necessary. I strive to balance modern technology with the ancient midwifery practices of my Native American ancestors.
Certifications
2009 to present: certification from the North American Registry of Midwives (NARM) as a Certified Professional Midwife (CPM).
1996 to present: certification/recertification in Neonatal Resuscitation by American Heart Association.
1995 to present: certification/recertification in CPR/Basic Life Support for Healthcare Providers by American Heart Association.
Philosophy
Birth is an intense, life-altering experience that changes a girl into a woman, a couple into a family and empowers a mother to nurture and defend her newborn. It is an honor and privilege to serve women and families during this transformation.
Women's bodies are perfectly designed to give birth safely and efficiently. Excellent diet and healthy lifestyle are the best prevention of complications during pregnancy and birth. Pregnancy is the time to prepare for the intensity of labor and birth. The strength of the body during labor can be an enjoyable, satisfying experience.
Midwives have helped women to give birth continuously throughout history right down to today. Modern midwives may have more tools than the midwives in history, but women's bodies still give birth the same way.
All of the valid scientific studies show that for healthy women, homebirth with a trained midwife is as safe as hospital birth with a physician. Some studies show it to be safer! But the biggest difference in outcomes between the two is that homebirth tends to result in less birth trauma to both mother and baby, better bonding between mother and baby, and a higher successful breastfeeding rate.
I am philosophically and spiritually opposed to circumcision. Not only is it un-necessary cosmetic surgery, it is an assault that permanently altars the body of a non-consenting minor.
Calling
In 1990 I was at the library to find out what to expect at the hospital if I agreed to labor coach for a friend. I checked out the standard mainstream pregnancy manuals, plus one book that would change my life forever, In Labor: Women and Power in the Birthplace by Barbara Katz Rothman. I couldn't put that book down. The next day, I returned all the main-stream birth books and checked out the homebirth books, including Spiritual Midwifery by Ina May Gaskin and The Birth Book by Raven Lang. I was hooked.
Deborah in front of emergency
entrance of CASA Hospital.
|
Three years later, I gave birth to our first child, a daughter, "unassisted" in the small camping trailer we lived in. We wanted to use a midwife for that birth, but circumstances forced us to choose unassisted homebirth instead. Soon after, I joined Missouri Midwives Association and began to learn everything I could about birth and midwifery. I had a second "unassisted" birth in 1995, because baby came before the midwife arrived! My third baby was born at home with the help of a midwife in 1997. He weighed 10 pounds, 12 ounces, and got stuck at the shoulders (shoulder dystocia). I was so grateful to have a midwife there to free him!
Most of my experience and training is with homebirth. I began my apprenticeship in 1995, carrying my baby with me to prenatal visits and births. As part of my training, my preceptor emphasized continuity of care by having me follow one or two women at a time. I was required to attend every prenatal, birth and postpartum visit for these women. My study assignments consisted of researching the details of everything that happened with these women. After a couple years of this, I filled in the gaps by studying more rare conditions and complications.
In 2007, I volunteered at CASA, a midwifery school and hospital in the state of Guanajuato, Mexico. It is kind of like a birth center, but also has hospital attributes in that the midwives can call in a doctor or surgeon if they need one, but he is not waiting in the next room. The school trains women to become Professional Midwives, so they can return to their communities and serve the women there. While there, I worked with the midwives in the hospital and met many amazing women. One of the students I met will return to her home in Guatemala and become the first Professional Midwife there!
Hablo un poco Espa�ol, and I know a little sign language (SEE).
I am a follower of Jesus Christ. I serve Christians, Pagans, Wiccans, Quiverful, Hippies, Rainbow, wealthy, poor, married, partnered, single, and everyone in-between. I am pleased to be able pass on the loving, quality care I received during my pregnancies and births.

